353 Middlestone
Way Cuyahoga
Falls, OH 44223 +1 (866)
796-0858
No matter what the specialty is, medical billing and coding are filled with numerous complexities. However, what sets the practice of Urology apart is the frequent changes in the ICD and CPT codes.
Handling the constantly evolving guidelines along with the healthcare practice is the main reason for the stress of urologists. Keeping up with codes and terminologies is a task that is vital to enhancing the financial performance of the practice.
As a urologist, losing track of the revenue cycle will lead to huge revenue losses. To prevent this, there is a need to stay adept with the steps in the billing process and streamline it to attain efficiency.
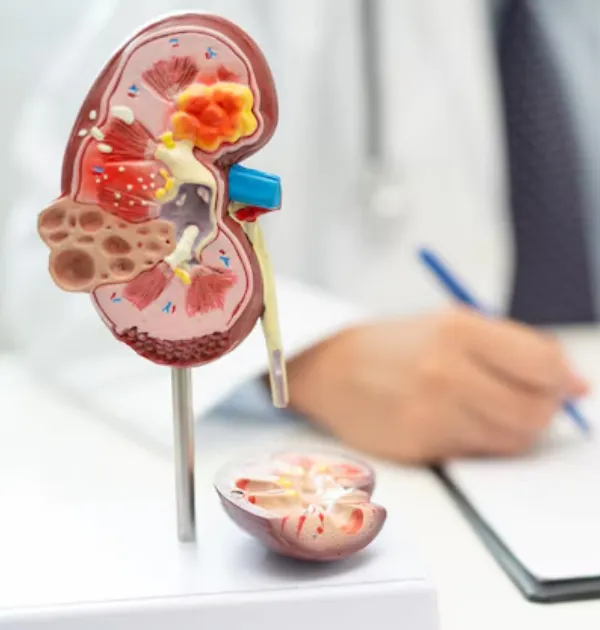
Managing the administrative part of a Urology practice requires in-depth knowledge and an outsourcing partner who provides effortless revenue cycle management services can handle it well. The skills of industry experts are valuable when it comes to CPT coding for Urology surgeries like:
Moreover, the ICD codes used are at par with the LCD guidelines. With a dedicated approach, an outsourcing partner can eliminate claim denials with efficient denial management.
By applying the best practices, your billing partner will boost the financial posture of the practice with timely reimbursement.

Cost to Collect Reduced by
Client Revenue Increased by
Happy Client
Collection Rate
Get in touch with us and ensure a healthcare practice that is never short of revenue and is always up to deliver the best care to the patients.
